The Mental Health Crisis in America
Mental illness and homelessness are deeply embedded in America. The connection between the two is complicated and has reciprocal effects on each other; that is, a person is likely to end up being homeless if his mental ability to carry out everyday lives becomes difficult, and if a person is homeless, he is likely to develop mental illness because of severe living conditions on the streets.
A Brief History of Homelessness in the United States
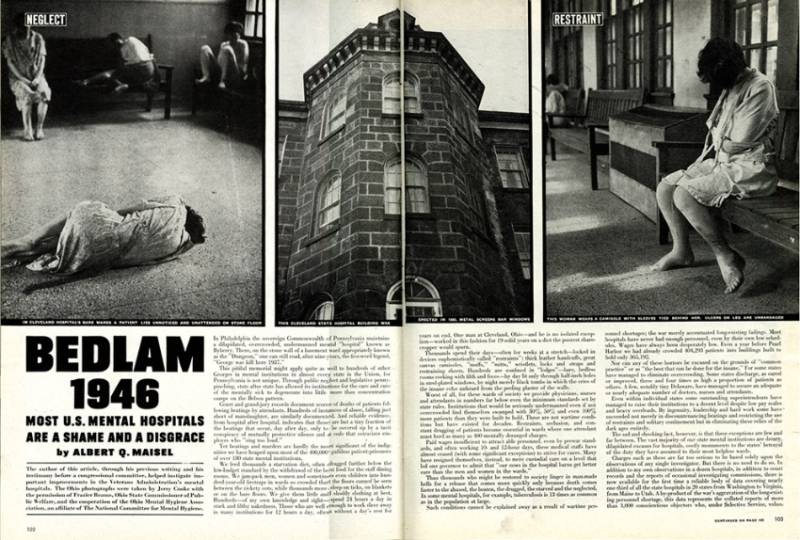
Homelessness in the United States has its roots in the late 19th and early 20th centuries when mass migration was common for workers. Teresa Gowan, the author of Hobos, Hustlers, and Backsliders: Homeless in San Francisco, explains that impoverished workers who lived on the roads and railways (without homes) became the first to be known as society’s homeless (3). Gowan further claims the country saw a spike in homelessness during the Ronald Reagan administration’s deinstitutionalization, or closure of state mental health hospitals. Along with Reagan’s social welfare rollback, deinstitutionalization led to discharge of thousands of mentally ill patients out in the community. While this movement was to stop involuntary hospitalization, cities all over America lacked funds to offer psychiatric services and often times, many mentally ill patients ended on the streets or in jails (4-6).

The Mental Health Crisis in California and San Francisco Today
In California, it is almost impossible to address the homeless crisis without acknowledging the mental health crisis. Phillip Reese wrote in “California Hospitals See Massive Surge in Homeless Patients” in Kaiser Health News, that more than 1/3 of 100,000 homeless patient visits to California hospitals in 2017, comprised of individuals with mental illness. Reese named San Francisco as one of the top counties that had the highest proportion of discharges involving homeless patients with mental health diagnosis. Erin Allday, a health care journalist who wrote a San Francisco Chronicle, “The Street’s Sickest, Costliest: The Mentally Ill,” also reported that 1/3 or more homeless in San Francisco are mentally ill who suffer mostly from post-traumatic stress, schizophrenia and bipolar disorder. Allday said mental health is “the most stubborn obstacle to San Francisco’s homelessness,” and called for a need for a reform in the mental health care system to stop the vicious cycle of streets, emergency rooms and jails.
What is Wrong with Mental Health Care System for Homeless People in San Francisco
In San Francisco, the mental health crisis is also visible on the streets and there is a clear need for a better mental health care system. In a San Francisco Chronicle article, “Fixing San Francisco’s Behavioral Health System is Complicated-Here’s Why,” Trish Thadani, a City Hall reporter, reported that the City spends about nearly $400 million on behavioral health services and 300 programs yet there seems to be unrelenting numbers of mentally distressed homeless people who have nowhere to go. Thadani named city’s mental health care system, a “tangled web of complex and expensive services,” which finally led Mayor Breed to appoint the city’s first Director of Mental Health Reform on March 27, 2019 (Thadani).
However, the city lacks many resources in the mental health care system. Performance Audit of the Department of Public Health Behavioral Health Services in April 2019 showed following findings:
- 90 % of 44,809 clients accessing psychiatric emergencies in 2016-2017 often have dual mental health and substance abuse disorders and experience homeless
- Nearly 40 % of 6,704 homeless people discharged from psychiatric emergency rooms were not contacted with follow up medical services in 2017. Linking them to services on discharge is important so they don’t “decompensating mentally, but of also resorting to alcohol and substance abuse after being discharged.”
- There is shortage of intensive care managers who are responsible for keeping clients engage in treatment and transition into community- “demand exceeds supply”
- There is a “constant presence of waitlists and wait times” for clients with substance use disorder. The average wait time is 5-21 days for residential non-methadone treatment and 1.3-66 days for outpatient non-methadone treatment in 2016.
Along with these findings, the city lacks beds in many facilities. Heather Knight, a columnist writing out of City Hall and the author of the San Francisco Chronicle, “A Glimmer of Hope for Mental Health Services in SF,” reported that there are too few beds in every level of care from emergency rooms, acute care to long term facilities. She also disclosed that psychiatric emergency room at SF General Hospital also has 18 beds yet there were 26 patients crammed in every corner of the facility on one Monday morning in 2019, and doctors often have to turn patients back quickly to the streets because of lack of long term care facilities.
The city also suffers from lack of interim places between psychiatric emergency and the streets such as transitional homes. Nuala Sawyer, the author and the news editor of San Francisco Weekly who wrote “Mental Health, Homelessness and Civil Rights: S.F.’s Crisis of Conscience,” stated that “all the shelters, transitional homes are always full,” and Hummingbird Place, San Francisco’s only behavioral health navigation center has 29 beds and they are constantly full.
It is apparent that homeless individuals frequent psychiatric emergencies the most but there is a clear lack of resources to support them despite the city’s spending on behavioral health services. If there are not enough beds in facilities, homeless individuals with mental disorder are likely to return to the streets without proper treatment. If these homeless individuals do not receive follow up services after their discharge due to lack or resources, there is a high chance that they will be back on the streets while their conditions worsen. These findings all signify that the homeless crisis in San Francisco is not solely about lack of affordable housing. Lack of an organized system in the mental health care services, as well as resources add complexity to the homeless population who are mentally distressed.
Mayor Breed’s solution to the mental health crisis on the streets

In an effort to address such mental and homeless crisis, San Francisco Mayor London Breed came forward with a proposition. In her Medium Blog post “280 New Navigation Center Beds and Continuing our Progress on Homelessness,” Mayor Breed proposed a solution to alleviating the mental health crisis – to- implement Senate Bill 1045 (SB 1045). Senate Scott Wiener authored SB 1045 and it grants an authority to San Diego, San Francisco and Los Angeles to “conserve” those who are suffering from mental illness and drug addiction in 5 year pilot program (Lipscomb). The term “conserve” takes the meaning of “institutionalization” where an individual is locked up in psychiatric facilities (Sawyer). California Governor Jerry Brown signed SB 1045 in September 2018, and each county can decide whether to implement the bill as long as each county can provide evidence that it has enough housing and medical services to those who are conserved (Sawyer). In San Francisco, a hearing is scheduled on May 14, 2019 at the Senate Appropriations Committee before the Board of Supervisors of San Francisco can implement this bill (Sawyer).
However, there is much controversy among civil rights group and people who claim that SB 1045 is not an effective solution to the underlying problem of homelessness because there is clearly a lack of mental health systems and NOT a lack of authority to detain those with mental illness. Instead of implementing Senate Bill 1045, Mayor Breed must alleviate San Francisco’s homeless crisis by reorganizing and increasing resources to improve the existing mental health care system.
Works Cited
Gowan, Teresa. Hobos, Hustlers, and Backsliders: Homeless in San Francisco. University of Minnesota Press, 2010.
Reese, Phillip. “California Hospitals See Massive Surge in Homeless Patients.” Kasier Health News, 2 April 2019. https://khn.org/news/california-hospitals-see-massive-surge-in-homeless-patients/
Allday, Erin. ” The Street’s Sickest, Costliest: The Mentally Ill.” San Francisco Chronicle, 26 June 2016. https://projects.sfchronicle.com/sf-homeless/mental-health/
Thadani, Trish. “Fixing San Francisco’s Behavioral Health System is Complicated-Here’s Why.” San Francisco Chronicle, 12 April 2019. https://www.sfchronicle.com/politics/article/Fixing-San-Francisco-s-behavioral-health-system-13761497.php
San Francisco Board of Supervisors, Budget and Legislative Analyst. Performance Audit of the Department of Public Health Behavioral Health Services. 19 April 2018.
https://sfbos.org/sites/default/files/041918_SF_MA_Behavioral_Health_Services.pdf
Knight, Heather. “A Glimmer of Hope for Mental Health Services in SF.” San Francisco Chronicle, 12 Feb 2019. https://www.sfchronicle.com/bayarea/heatherknight/article/A-glimmer-of-hope-for-mental-health-services-in-SF-13608554.php
Lipscomb, Kathy. “Open Forum: Why San Franciscans Must Support Housing Conservatorships.” San Francisco Chronicle, 28 Feb 2019. https://www.sfchronicle.com/opinion/openforum/article/Open-Forum-Why-San-Franciscans-must-support-13650741.php
Sawyer, Nuala. “Mental Health, Homelessness, and Civil Rights: S.F’s Crisis of Conscience.” San Francisco Weekly, 20 Mar 2019.
http://www.sfweekly.com/news/mental-health-homelessness-and-civil-rights-s-f-s-crisis-of-conscience/
Breed, London. “280 New Navigation Center Beds and Continuing Our Progress on Homelessness.” Medium, 8 March 2019,
https://medium.com/@LondonBreed/280-new-navigation-center-beds-and-continuing-our-progress-on-homelessness-abe418bba869
This is the Part 1 of 4. For the next part, please click here
The pictures speak for themselves . So heartbreaking. I hope the proposal will pass and people in need will be helped.
LikeLike
this is a great topic, great information. I do wish you covered how many homeless people are drug addicts. I think that would be a very vital source of data.
LikeLike
I like how you connected mental illnesses and homelessness. Great information, especially when you pointed out how World War II contributed to the homelessness. Soldiers suffering from PTSD, were unable to continue to live a normal life, so they became homeless.
LikeLike
This is terrific thanks for hitting the head on the nail on this one!
LikeLike
Difficult topic. Will there every be a solution for homelessness? I hope so! SF has the money and it should go to this IMPORTANT issue!
LikeLike
It’s so challenging to find solutions to help those experiencing homelessness, but then when mental health challenges are present, it complicate things further. It’s challenging to find a solution that is both empowering and meaningful.
LikeLike
People struggling with mental health and experiencing homeless need unique solutions. A broken health care system exacerbates the problem. Why aren’t there more case managers and more substance abuse treatment beds – because of funding. The funding is limited and doesn’t pay rates high enough to maintain a strong workforce to address mental health. Much of this is caused by low Medicaid rates, but it’s also because all types of insurance, commercial included, place unrealistic limitations on mental health providers. Just because you get an assessment that says you need mental health or substance abuse treatment doesn’t mean your insurance will pay for it.
In Hawaii the state is also debating laws for longer periods of involuntary psychiatric admissions. It’s a difficult balance between individual patient rights and protecting people in crisis. When people are in crisis with suicidal ideation or experiencing delusions they may not have the capacity judge what is necessary to get well. A 48 hour hold now allowed in Hawaii is often not enough time for people to stabilize, particularly for those with little to no family support and resources. Here’s an article about some of what’s being discussed in Hawaii you might be interested in. https://www.civilbeat.org/2019/03/bill-focuses-on-revolving-door-of-involuntary-psychiatric-treatments/
LikeLike